Trichinella Spiralis
Trichinellosis is a cosmopolitan parasitic disease due to nematodes of the Trichinella genus, constituted of twelve different taxa. Humans are a parasitical deadlock and get infected by ingestion of raw or undercooked meat that contain infesting larvae (Pozio et al., 2013).
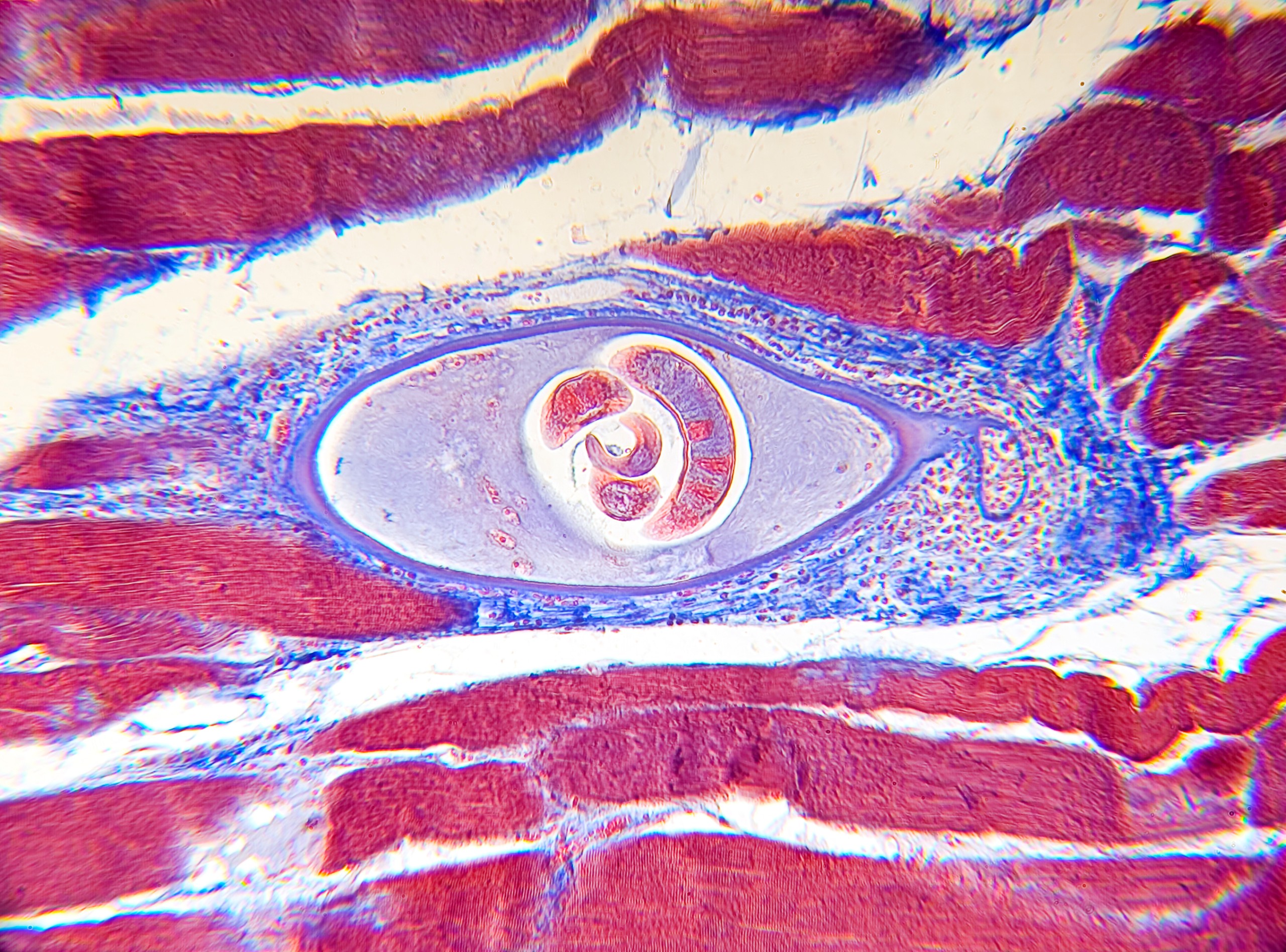
This viviparous parasite has the particularity to accomplish its whole cycle within a single host. L1 infesting larvae released during digestion rapidly become adult after 4 months. Every fertilized female release between 500 to 1000 larvae. They migrate through blood and lymphatic streams in the entire organism to reach highly oxygenated muscles, where they become encapsulated. Encapsulated larvae can then divert the metabolism of striated muscle cells allowing them to survive for years.
More than 150 mammalian and bird species can host Trichinella larvae in their muscles. Pigs are the main players of the domestic cycle, even though this transmission mode has been decreasing in countries where hygiene is better controlled. Boars are responsible of small outbreaks, especially in France. Other outbreaks due to horse meat have been observed as well, in countries where the meat is eaten raw or undercooked (France, Italy…) (Gottstein et al., 2009). Clinical manifestations usually occur in 4 stages: a short invasion phase with diarrhea within the 12 to 48 first hours, followed by a digestive incubation stage that takes 1 to 3 weeks, an acute phase with fever, myalgia, face edema, asthenia and sometimes complications, and, finally, a recovery stage.
Death is possible in case of sepsis or visceral failure due to larvae encapsulated in these organs. Sequelae may occur when the Central Nervous System or the heart are affected. Asymptomatic or subclinical forms are observed, most commonly due to minimal parasitic infections (Diaz et al., 2020). Diagnosis based on clinical, epidemiological and biological (hypereosinophilia, elevated muscular enzymes) data has to be confirmed by serology and muscular biopsy. However, biopsies are invasive and may be source of false negative results. Once the diagnosis is certain for one patient of an epidemic cluster, the diagnosis of the other patients can rely on the sole serology (Bruschi et al., 2019).
Amongst serological techniques, Immunofluorescence and ELISA are the most commonly used. However, they may lack sensitivity and specificity due to the purification quality of the antigen. Total larva antigens can show cross-reactions with other nematodes or autoimmune diseases, while Excretory/Scretory antigens lack sensitivity during the first months of infection (Barennes et al., 2008).
SCIENTIFIC REFERENCES
- Andiva S, Yera H, Haeghebaert S, Tourte-Schaefer C, Magnaval JF, Dupouy-Camet J. Comparative evaluation of a latex agglutination test, two Elisa tests and a Western blot test for the serodiagnosis of human trichinellosis. 2002; Ann Biol Clin (Paris). 60(1):79-83
- Barennes H, Sayasone S, Odermatt P, De Bruyne A, Hongsakhone S, Newton PN, et al. A major trichinellosis outbreak suggesting a high endemicity of Trichinella infection in northern Laos. 2008 Jan; J Trop Med Hyg. 78(1):40–4.
- Dorny P, Praet N, Deckers N, Gabriel S. Emerging food-borne parasites. Vet Parasitol. 2009 Aug 7;163(3):196–206.
- Dupouy-Camet J. Trichinellosis: still a concern for Europe. Eurosurveillance. 2006 Jan 1;11(1):3–4.
- Dupouy-Camet J, Talabani H, Ancelle T. Trichinellosis. 2010; Rev Prat 60(2) :159‑164
- Gottstein B, Pozio E, Nöckler K. Epidemiology, diagnosis, treatment, and control of trichinellosis. 2009; Clin Microbiol Rev. 22(1):127-145.
- Nöckler K, Reckinger S, Broglia A, Mayer-Scholl A, Bahn P. Evaluation of a Western Blot and ELISA for the detection of anti-Trichinella-IgG in pig sera. 2009 Aug 26; Vet Parasitol. 163(4):341–7
- Pozio E. The opportunistic nature of Trichinella–exploitation of new geographies and habitats. 2013 May 20; Vet Parasitol. 194(2–4):128–32.
- Pozio E. World distribution of Trichinella spp. infections in animals and humans. 2007 Oct 21; Vet Parasitol. 149(1–2):3–21.
- Pozio E, Zarlenga DS. New pieces of the Trichinella puzzle. 2013 Nov; Int J Parasitol. 43(12–13):983–97.
- Rainova I, Kaftandjiev I, Harizanov, R, Tsvetkova N, Jordanova D, Marinova I. Outbreaks of human trichinellosis, still a challenge for the public health authorities in Bulgaria. 2016 August; J Pub Health 24(4):291–297.
- Yera H, Andiva S, Perret C, Limonne D, Boireau P, Dupouy-Camet J. Development and Evaluation of a Western Blot Kit for Diagnosis of Human Trichinellosis. 2003 Sep; Clin Diagn Lab Immunol. 10(5):793–6.
- Yera H, Mergey T, Limonne D, Lureau P, Dupouy-Camet J. Seroprevalence of Trichinella antibodies in blood donors in France. 2011; 13th ICT (Int. Conf. on Trichinellosis), Changchun, China.
{{ productCount ? productCount : 'Showing all 4 results' }}




